Vitamin B3
Vitamin B3 is used by cells to make the essential cofactor, nicotinamide adenine dinucleotide (NAD+). All forms of life use NAD+ in reactions in cells to make energy. All lifeforms require NAD+ to sustain life. [1]
Supplementation with vitamin B3 has become a valuable nutritional and therapeutic strategy. Suboptimal levels of vitamin B3 yield cellular dysfunction. Short-term vitamin B3 deficiency leads to pellagra.[1][2][3] Pellagra is a deadly and debilitating disease, occurring in regions in the world with severe malnutrition. In developed regions of the world, vitamin B3 deficiency occurs due to poor dietary choices, alcoholism, and infectious or autoimmune diseases.[4][5][6][1][7] Some symptoms of vitamin B3 deficiency include diarrhea, skin irritation, depression, fatigue, and headache.
Protection against pellagra comes from consumption of B3 vitamin sources. In 1915, American doctor, Joseph Goldberger, discovered pellagra results from malnutrition. Goldberger found pellagra could be prevented with diets containing B3 vitamins in yeast, eggs, peanuts, meat, and cereals.
Contents
Forms Vitamin B3
Niacin (NA) and nicotinamide (NAM) are B3 vitamins which the body can use to synthesize NAD+. The body can also use the protein building block, the amino acid tryptophan, to synthesize NAD+. Other B3 vitamins include the supplements, nicotinamide mononucleotide (NMN) and nicotinamide riboside (NR).[8]
Vitamin B3 intake
In the United States, the recommended intake of niacin is 14 mg per day in adult women and 16 mg per day in adult men.[9] Consuming higher doses of B3 vitamins can have protective effects in some diseases.
Beneficial effects of Vitamin B3
In diabetes, a high dose of nicotinamide (25-50 mg per kg) has been shown to protect pancreas cells. A high dose of nicotinamide has also been shown to provide protection to neurons in fetal alcohol syndrome. In patients with high cholesterol, high doses of nacin were shown to reduce fats in the blood, reduce numbers of death, and to reduce numbers of heart complications.[10]
Adverse effects of vitamins B3
The most common symptoms from consuming low doses (50-500 mg) of niacin are flushing (itching, warmth, or tingling), abdominal pain, headache, diarrhea, indigestion, nausea, vomiting, and rash. These effects can be avoided with using lower dosages and increasing the dosage gradually. These adverse effects can also be avoided if niacin is not taken on an empty stomach.[11]
High-dose niacin therapy (1-3 grams per day) is used to treat low blood pressure, fatigue, insulin resistance, heartburn, and blurred or impaired vision. Side effects of long-term, high dosage use include liver dysfunction, hepatitis, and liver failure.9 Taking niacin at high doses long-term also increases the risk of brain stroke and hemorrhage, ulcers and bleeding, diabetes, indigestion, and diarrhea.[11]
Food sources of vitamin B3
Vitamin B3 can be found in food sources in the forms of both niacin and nicotinamide.[12]
Food sources of nicotinamide
Meat, fish, nuts, and mushrooms contain nicotinamide in trace amounts. An even lesser amount of nicotinamide is available in some vegetables. B3 vitamin supplements also contain 20-30mg of nicotinamide.
Food sources of niacin
| Source | Serving | Niacin |
|---|---|---|
| Chicken | 3 ounces | 8.9 mg |
| Tuna (canned) | 3 ounces | 8.6 mg |
| Turkey | 3 ounces | 9.9 mg |
| Salmon | 3 ounces | 8.5 mg |
| Beef | 3 ounces | 4.4 mg |
| Cereal (unfortified) | 1 cup | 6.3 mg |
| Cereal (fortified) | 1 cup | 23.5 mg |
| Peanuts (dry-roasted) | 1 ounce | 4.1 mg |
| Pasta (enriched) | 1 cup | 2.2 mg |
| Lentils | 1 cup | 2.1 mg |
| Lima beans | 1 cup | 2.1 mg |
| Bread (whole-wheat) | 1 slice | 1.4 mg |
| Coffee | 1 cup | 2.0 mg |
Vitamin B3 biosynthesis to NAD+
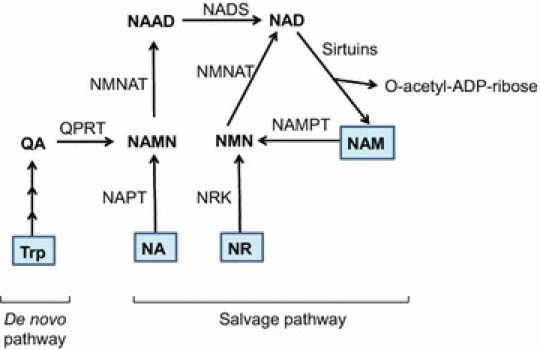
Niacin can contribute to NAD+ biosynthesis through entering the salvage pathway. Niacin converts to NAMN via the enzyme, NAPT. Nicotinamide, the other B3 vitamin, can enter the NAD+ biosynthesis pathway as well. It enters the recycling pathway of the salvage pathway of NAD+ biosynthesis. Nicotinamide is converted to NMN via the enzyme, NAMPT.
Tryptophan, the protein building block, can enter the NAD+ biosynthesis pathway through the de novo pathway of NAD+ synthesis. In this manner, tryptophan from meats can also lead to the synthesis of NAD+.[13]
B3 vitamins and their product of biosynthesis, NAD+, are tightly connected to metabolism. Metabolism has a special role in the aging processes of mammals. Organism aging entails time and maturation culminating in cell, tissue, and organism death. Two key factors play roles in aging: accumulation of random changes and genes altering lifespan. NAD+ plays a vital role in the random changes of aging and also in the genetic, programmed aspects of aging. NAD+ maintains the transfer of electrons in cellular reactions, regulates calcium storage, regulates DNA damage and repair, and energy metabolism.[14]
B3 vitamins can stimulate cellular activity on their own, and cells can use them to synthesize NAD+. B3 vitamins can also inhibit cell signaling enzymes. The B3 vitamin deficiency-induced disease, pellagra, highlights the importance of B3 vitamins in maintaining human health. Cells biosynthesize NAD+ from B3 vitamins through multiple biosynthetic pathways, highlighting its crucial role in cellular metabolism and health. An enzyme adds a phosphate group in cells to NAD+, producing NADP. NADP gains electrons to generate NADPH. NADPH can then give electrons to molecules or ions in cells to protect against cell stress in aging. Depletion of NAD+ during aging can inhibit the activity of NADPH, which has adverse effects on healthy aging.
Biosynthesis of NAD+ with B3 vitamins can stimulate sirtuins, proteins involved in DNA repair and chromosome stability. NAD+ also acts as a molecule which PARPs use for their function. PARPs repair damaged DNA during aging. Enzymes involved in immune system function, CD38, use NAD+ for their functions during aging as well.
References
- ↑ 1.0 1.1 1.2 Mikhail V Makarov, Samuel AJ Trammell, Marie E Migaud. The chemistry of the vitamin B3 metabolome. Biochem Soc Trans, 2018; DOI: 10.1042/BST20180420.
- ↑ LJ Hill, AC Williams. Meat intake and the dose of vitamin B3—nicotinamide: cause of the causes of disease transitions, health divides, and health futures? Int J Tryptophan, 2017; DOI: 10.1177/11778646917704662.
- ↑ S Srivastava. Emerging therapeutic roles for NAD(+) metabolism in mitochondrial and age-related disorders. Clin Transl Med, 2016; DOI: 10.1186/s40169-016-0104-7.
- ↑ MA Crook. The importance of recognizing pellagra (niacin deficiency) as it still occurs. Nutrition, 2014; DOI: 10.1016/j.nut.2014.03.004.
- ↑ A Garrido, N Djouder. NAD+ deficits in age-related diseases and cancer. Trends Cancer, 2017; DOI: 10.1016/j.trecan.2017.06.001.
- ↑ R Li, K Yu, Q Wang, L Wang, J Mao, J Qian. Pellagra secondary to medication and alcoholism: a case report and review of the literature. Nt Clin Pract, 2016; DOI: 10.1177/0884533616660991.
- ↑ N Terada, K Kinoshita, S Taguchi, Y Tokuda. Wernicke encephalopathy and pellagra in an alcoholic and malnourished patient. BMJ Case Rep, 2015; DOI: 10.1136/bcr-2015-209412.
- ↑ Antony A Sauve. NAD+ and vitamin B3: From metabolism to therapies. J Pharmacol Exp Ther, 2008; DOI: 10.1124/jpet.107.120758.
- ↑ Institute of Medicine (1998). "Niacin". Dietary Reference Intakes for Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline. Washington, DC: The National Academies Press. pp. 123–149. ISBN 978-0-309-06554-2. Retrieved 7 April 2020.
- ↑ Niaspan® (niacin extended-release) tablets prescribing information. AbbVie Inc., US-NIAS-180036, North Chicago, IL 60064 December 2018.
- ↑ 11.0 11.1 "Niacin Fact Sheet for Health Professionals". 15 January 2019. Retrieved 7 April 2020.
- ↑ “Niacin.” lpi.oregonstate.edu/mic/vitamins/niacin. Retrieved 7 April 2020.
- ↑ S Srivastava. Emerging therapeutic roles for NAD(+) metabolism in mitochondrial and age-related disorders. Clin Transl Med, 2016; DOI: 10.1186/s40169-016-0104-7.
- ↑ Ping Xu, Anthony A Sauve. Vitamin B3, the nicotinamide adenine dinucleotides and aging. Mech Ageing Dev, 2010; DOI: 10.1016/j.mad.2010.03.006.